Capitol Insights Newsletter
Authors: Luke Schwartz, Parker Krex, and Matt Reiter
What happened in Congress this week?
Congress was out of session this week.
MedPAC Releases June Report and its 2024 Data Book
Last month, MedPAC released its June Report. MedPAC publishes two reports a year, one in March and a second in June. These reports provide an overview and analysis of the status of the Medicare program and offer policy recommendations to Congress.
June’s report covered a wide range of issues, including provider payment reform, incentivizing participation in advanced alternative payment models, and issues within Medicare Advantage (MA).
The report carried a message similar to MedPAC’s previous reports: physicians’ input costs are rapidly increasing faster than updates to the Medicare Physician Fee Schedule (PFS). The report highlighted the growing gap between PFS updates and the Medicare Economic Index (MEI). It made clear that the payment problems providers are currently experiencing will continue to worsen without Congressional action. The Report also cautioned that increasing medical inflation “could create incentives for clinicians to reduce the number of Medicare beneficiaries they treat or stop participating in Medicare entirely.”
To exacerbate current problems, the Commission expressed concern about the upcoming sunsetting of participation bonuses for clinicians in alternative payment models, which are larger than the biggest adjustments available through the Merit-based Incentive Payment System (MIPS). The report identified several solutions utilizing alternative payment models to address the physician payment problems.
One approach offered by the Commission is to update total PFS payment rates by the MEI minus 1 percentage point. This approach reflects the historical average of PFS updates, which have been around MEI minus 1 percentage point for the last 20 years. MedPAC identified this as the simplest and most effective path forward for addressing falling physician payments.
Another main talking point of the report is Medicare Advantage. While the June MedPAC report did not offer any official recommendations, it emphasized the need to create a national provider directory to increase transparency surrounding the network adequacy of MA plans. Furthermore, the report reiterated the importance of easing the provider burden associated with prior authorization requests. The report cited a study showing the drastic increase in prior authorization requests that physicians have to deal with daily—a burden that is both costly and distracts physicians from patient care.
The Report also highlighted inaccuracies in MA data, specifically encounter data and reported data. The Commission showcased the usefulness of the missing data, especially to Congress, to better understand and improve MA. Because of the missing encounter data, other data set conclusions may be inaccurate, or incomplete. The areas with the greatest data discrepancies are inpatient services, dialysis, skilled nursing, and home health services.
As for data submitted by MA plans, the data is sometimes rejected by CMS and never published. Therefore, it is unclear if missing reporting data is from being rejected or not being published. MedPAC is worried about inefficiencies in data reporting as it makes it harder to study and investigate the failures and successes of MA.
Relatedly, MedPAC released some supporting data in its 2024 Data Book earlier this week.
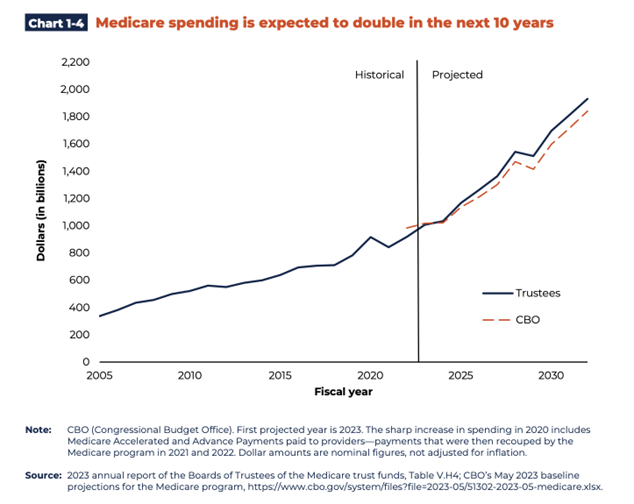
Overall, the data demonstrates that MA plans are continuing to grow in popularity as people transition from traditional fee for service (FFS) into MA plans. The data also shows that Medicare spending continues to grow rapidly and is expected to double in the next 10 years.
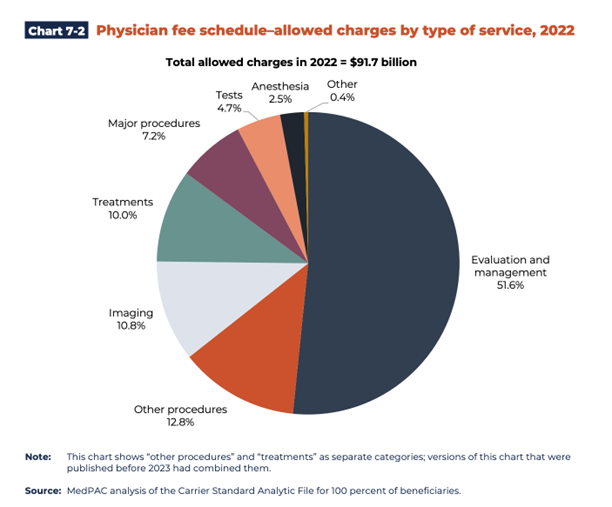
The data also presents data related to the fee schedule. For example, Chart 7-2 below shows that Evalution and Management (E&M) services account for over half of Medicare allowed charges.
The data provides helpful insights into many of the topics covered in MedPAC’s two official reports this year.
Top Stories in Healthcare Policy
The FTC is investigating DaVita and Fresenius Medical Care, the nation’s two largest dialysis providers. The probe is over their alleged actions to hurt smaller competitors.
The House GOP HHS Appropriations report lays out stances against drug march-ins, drug negotiation, and proposes to reform 340B. The appropriations bill is unlikely to pass the senate or become law in its current form.
CMS has released guidance to help people with Medicare prescription drug coverage pay out-of-pocket costs in monthly installments. The Medicare Prescription Payment Plan launches next year.
A group of 138 hospitals have filed a lawsuit against the Biden Administration. The hospitals are challenging what they say are permanent cuts to their Medicare payments.
A report from the Manhattan Institute questions the healthcare system’s role in addressing social determinants of health.